Clay Christensen, Jerome Grossman and Jason Hwang on Intuitive Medicine vs. Precision Medicine
I found the passage below from The Innovator’s Prescription (location 333), by Clay Christensen, Jerome Grossman and Jason Hwang especially insightful. It puts diagnosis at the center of medicine, especially when viewing medicine from a business point of view. Better and better diagnosis opens up the possibility of more cost-efficient treatments for those diseases that are precisely identified. But that possibility must be seized.
Our bodies have a limited vocabulary to draw upon when they need to express that something is wrong. The vocabulary is comprised of physical symptoms, and there aren’t nearly enough symptoms to go around for all of the diseases that exist—so diseases essentially have to share symptoms. When a disease is only diagnosed by physical symptoms, therefore, a rules-based therapy for that diagnosis is typically impossible—because the symptom is typically just an umbrella manifestation of any one of a number of distinctly different disorders.
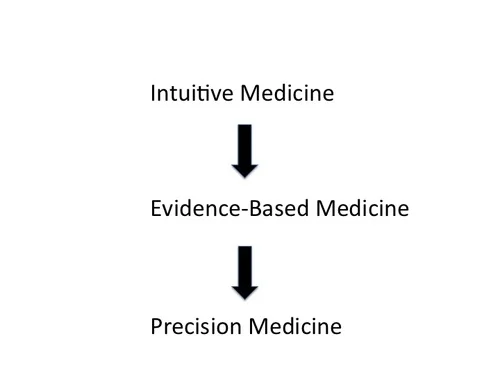
The technological enablers of disruption in health care are those that provide the ability to precisely diagnose by the cause of a patient’s condition, rather than by physical symptom. These technologies include molecular diagnostics, diagnostic imaging technology, and ubiquitous telecommunication. When precise diagnosis isn’t possible, then treatment must be provided through what we call intuitive medicine, where highly trained and expensive professionals solve medical problems through intuitive experimentation and pattern recognition. As these patterns become clearer, care evolves into the realm of evidence-based medicine, or empirical medicine—where data are amassed to show that certain ways of treating patients are, on average, better than others. Only when diseases are diagnosed precisely, however, can therapy that is predictably effective for each patient be developed and standardized. We term this domain precision medicine.
… disruption-enabling diagnostic technologies long ago shifted the care of most infectious diseases from intuitive medicine (when diseases were given labels such as “consumption”) to the realm of precision medicine (where they can be defined as precisely as different types of infection, different categories of lung disease, and so on). To the extent that we know what type of bacterium, virus, or parasite causes one of these diseases—and when we know the mechanism by which the infection propagates—predictably effective therapies can be developed—therapies that address the cause, not just the symptom. As a result, nurses can now provide care for many infectious diseases, and patients with these diseases rarely require hospitalization. Diagnostics technologies are enabling similar transformations, disease by disease, for families of much more complicated conditions that historically have been lumped into categories we have called cancer, hypertension, Type II diabetes, asthma, and so on.
When I was a kid, we talked about “curing cancer” as the prototypical world-shaking accomplishment. The reason there is no one “cure for cancer” is that cancer is not one disease but hundreds of different diseases involving different genes going awry in the direction of too much growth. A cure needs to be found for each one of those diseases in order for there to be a cure for the amorphous notion of “cancer.” Many of these diseases have been cured and others are well on their way to being cured. But other diseases under the general heading of “cancer” have not even been identified yet (in the sense of carefully distinguishing them from other diseases with similar symptoms). Once they have been identified at the level of the particular gene that goes awry to produce that particular disease, they will be halfway to being cured.
The term “personalized medicine” is sometimes used for what I would call “treating the disease someone actually has instead of some other disease.” A better phrase for that is the phrase Clay, Jerome and Jason use: “precision medicine.”